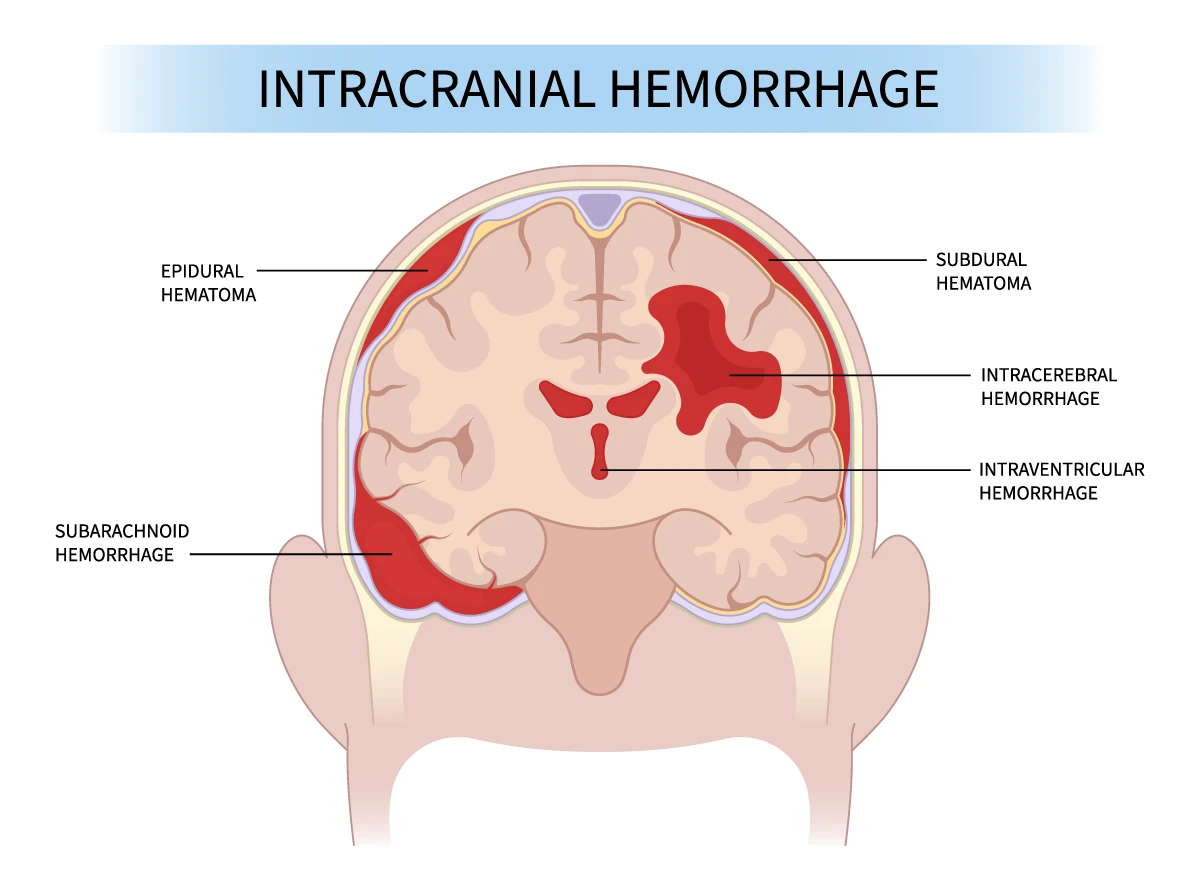
Intracerebral haemorrhage (ICH) is a serious and life-threatening condition that occurs when a blood vessel ruptures within the brain, leading to bleeding in the surrounding brain tissue. However, it can be treated with prompt and effective methods to improve outcomes and reduce the risk of long-term complications.
Here we explore the various options available for intracerebral haemorrhage treatment, the outcomes patients can expect, and how specialised care, like that provided at top institutions such as Nanavati Max Hospital, plays a critical role in managing this condition.
Understanding Intracerebral Hemorrhage
Intracerebral haemorrhage is often caused by high blood pressure, head trauma, aneurysms, or blood vessel abnormalities. The bleeding leads to increased pressure within the skull, which can cause significant damage to brain tissues. Symptoms of ICH may include sudden headache, weakness, numbness, vision changes, and difficulty speaking or understanding speech. Immediate medical attention is essential to minimise the impact of the haemorrhage on the brain.
Emergency Medical Care
- Initial Assessment and Stabilisation: When a patient presents with symptoms of an intracerebral haemorrhage, rapid assessment and stabilisation are crucial. Medical professionals will evaluate the patient’s vital signs, and neurological status, and perform imaging tests such as CT scans or MRIs to confirm the diagnosis and determine the extent of the bleeding.
- Blood Pressure Management: Controlling high blood pressure is a vital component of emergency treatment, as elevated blood pressure can exacerbate the bleeding. Medications are administered to lower blood pressure and reduce the risk of further haemorrhage.
- Airway Protection and Ventilation: In severe cases, patients may require assistance with breathing and airway protection to ensure adequate oxygen supply to the brain and prevent further complications.
Surgical Treatment Options
- Craniotomy: In cases where the haemorrhage is large or causing significant pressure on the brain, a craniotomy may be performed. This surgical procedure involves removing a portion of the skull to access the brain and evacuate the blood clot. Removing the clot can relieve pressure on the brain and prevent further damage.
- Minimally Invasive Surgery: Some patients may be candidates for minimally invasive surgical techniques, such as endoscopic or stereotactic surgery. These procedures use smaller incisions and specialised tools to remove the blood clot with minimal disruption to surrounding brain tissue.
- Hematoma Drainage: Another surgical option is the drainage of the hematoma (blood clot) through a small hole drilled in the skull. This procedure is less invasive and can be effective in reducing intracranial pressure in certain cases.
Non-Surgical Treatment Approaches
- Medical Management: In some cases, especially when the haemorrhage is small or located in an area that is difficult to access surgically, medical management may be the preferred approach. This includes controlling blood pressure, managing symptoms such as headaches or seizures, and monitoring the patient closely in a neuro-intensive care unit.
- Rehabilitation and Therapy: After the acute phase of treatment, rehabilitation is a crucial part of recovery. Patients may need physical therapy, occupational therapy, and speech therapy to regain lost functions and adapt to any residual disabilities caused by the haemorrhage.
- Medications: Patients may be prescribed medications to prevent complications, such as anticoagulants to manage blood clotting disorders or anticonvulsants to prevent seizures.
Advanced Imaging and Monitoring
- Continuous Monitoring: Advanced medical facilities, like those at Nanavati Max Hospital, often use continuous monitoring techniques to track a patient’s neurological status and intracranial pressure. This allows for early detection of any changes that may require intervention.
- Repeat Imaging: Regular imaging studies, such as follow-up CT scans or MRIs, are essential to monitor the progress of the haemorrhage and assess the effectiveness of the treatment. These imaging tests help guide ongoing treatment decisions and ensure the best possible outcomes for the patient.
Potential Outcomes and Recovery
- Factors Influencing Recovery: The outcome of intracerebral haemorrhage treatment depends on various factors, including the size and location of the haemorrhage, the patient’s overall health, and the speed of treatment. Early intervention and access to specialized care can significantly improve recovery prospects.
- Long-Term Rehabilitation: Patients recovering from ICH may require long-term rehabilitation to address any neurological deficits. This can include therapies meant to improve mobility, cognitive function, and speech, depending on the areas of the brain affected by the haemorrhage.
- Supportive Care: Ongoing supportive care, including nutritional support, psychological counselling, and caregiver education, is vital for helping patients and their families adjust to the changes brought about by the haemorrhage.
The Importance of Specialised Care
- Expertise in Neurocritical Care: Choosing a medical facility with expertise in neurocritical care is crucial for successfully treating intracerebral haemorrhage. Various hospitals offer access to highly skilled neurosurgeons, neurologists, and intensive care specialists experienced in managing complex cases of ICH.
- Multidisciplinary Approach: A comprehensive, multidisciplinary approach to treatment ensures all aspects of the patient’s care are addressed. This includes the acute management of the haemorrhage and long-term rehabilitation and follow-up care.
Patient and Family Education
- Understanding the Condition: Educating patients and their families about intracerebral haemorrhage, its causes, and the treatment options available is essential. This knowledge empowers them to make informed decisions and participate actively in the care process.
- Emotional and Psychological Support: Coping with the aftermath of an intracerebral haemorrhage can be challenging for both patients and their families. Access to counselling and support groups can provide emotional support and help them navigate the recovery journey.
Conclusion
Intracerebral haemorrhage treatment requires a multifaceted approach that combines prompt emergency care, surgical and non-surgical interventions, and long-term rehabilitation. With appropriate medical care, patients have a better chance of achieving positive outcomes and regaining their quality of life. If you or a loved one is facing an intracerebral haemorrhage, seeking specialised care and understanding the available treatment options can make a significant difference in the recovery process.